Schizophrenia is a mental health disorder that is chronic and disabling and affects the way a person thinks, feels, and behaves. Typically, symptoms start between the ages of 16 and 30; rarely it is observed in children as well.
Symptoms of this disease are categorized into 3 types – positive, negative, and cognitive:
Positive symptoms: These are symptoms that do not occur in healthy people.
– Hallucinations
– Delusions
– Thought disorders
– Movement disorders
Negative symptoms: These are characterized by disrupted normal thoughts and behavior.
– Flat affect
– Reduced feelings of pleasure
– Difficulty starting and continuing activities
– Diminished speech
Cognitive symptoms: These relate to the process of thinking.
– Poor executive functioning
– Trouble focusing
– Problems with working memory
In 1910, Swiss psychiatrist Paul Eugen Bleuler composed the term ‘schizophrenia’ from the Greek words ‘schizo’, meaning split, and ‘phren’, meaning mind. Some people have confused schizophrenia with multiple personalities but this was not Bleuler’s intent. He was aiming to replace the even more confusing term of ‘dementia praecox’, meaning dementia of early life. The previous term had been used by German psychiatrist, Emil Kraeplin, who mistaking believed that there was an inevitable mental deterioration. While he may have been incorrect in his beliefs, he is credited with being the first one to have delineated schizophrenia from other forms of psychosis in 1887.
In more ancient times, all forms of psychoses were indiscriminately referred to as “madness”. It was not even seen as a form of illness, but rather viewed as a divine punishment or demonic possession. It was not until 460-377 BC when Hippocrates brought mental illness under scientific scrutiny. It was in the 20th century that Sigmund Freud defined schizophrenia as unresolved conflicts starting in childhood. Many advances have been made since that time.
Approximately 21 million people around the world suffer from schizophrenia. It is somewhat more common in men and tends to start at an earlier age in men. Those suffering from schizophrenia are 2-2.5 times more likely to die at an early age than the rest of the population. Internationally, the prevalence of schizophrenia is close to 1%. The usual age of onset is adolescence and is rarely diagnosed past the age of 45. In the US, the prevalence is 0.3% in any given year. There is a 5% risk of suicide among those diagnosed with schizophrenia.
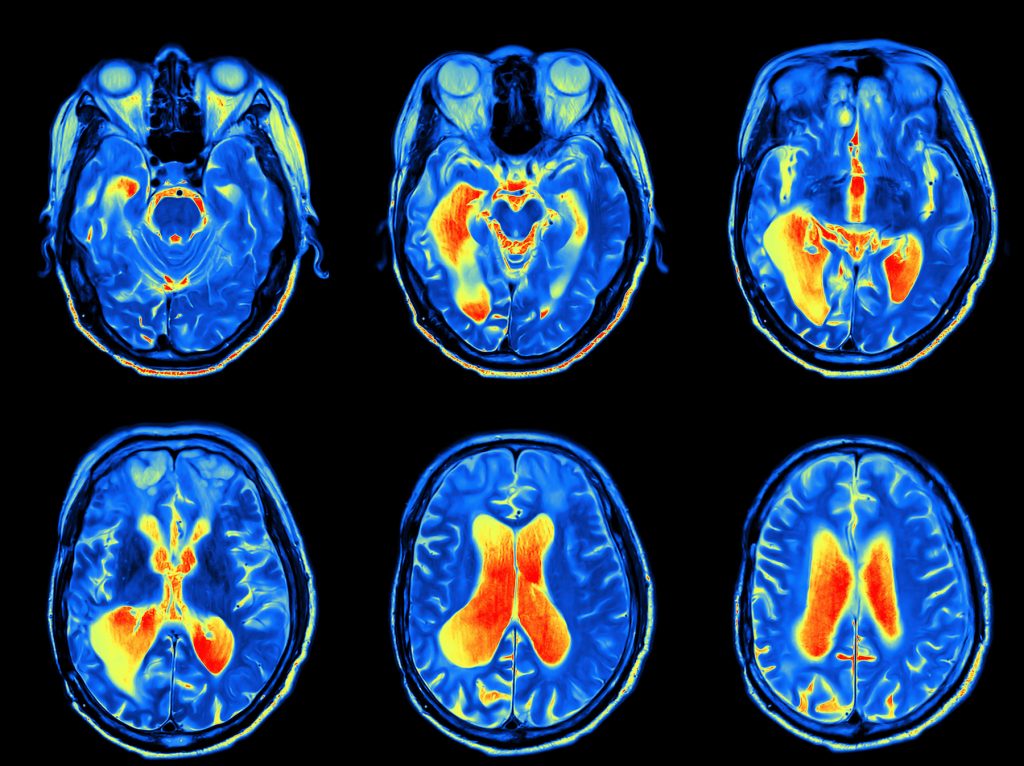
The neuropathologic findings have been controversial while the genetic mechanisms in play have been difficult to identify. Although brain volume and weight are reduced in patients with schizophrenia, there is an enlargement of the ventricles. Imaging studies suggest abnormalities in the hippocampus, neocortex, and thalamus. Some studies have demonstrated similar brain findings in relatives of a schizophrenic patient reinforcing genetic causes. One of the most interesting histological findings are clustered neurons in the lamina II of the entorhinal cortex and in the neocortical white matter. This suggests an early neurodevelopmental anomaly. Many twin studies have been conducted confirming the inheritability of this disease, with an approximate 80% risk.
In one study published in JAMA Psychiatry, it was noted that adult schizophrenic patients in the US had a 3.5 times higher death rate than the rest of the population. Despite the fact that suicide was more common in these patients, approximately 85% of these deaths were due to natural causes, most commonly cardiovascular and respiratory disorders. Of these natural deaths, cardiovascular diseases accounted for 1 out of every 3 mortalities. Among the unnatural deaths, suicide was responsible for 1 out of 4 and substance abuse 8.2%.
In another study published in the journal, Cancer, mortality data was analyzed on over 3.400 French patients over an 11 year timeframe. It was found that women with schizophrenia were twice as likely to die from cancer than the general population. Furthermore, breast cancer was almost 3 times higher in these patients. In men, lung cancer was almost twice as high as the general population but the mortality did not appear to differ significantly. It was postulated that schizophrenics are more likely to smoke and less likely to do cancer screening. The higher mortality rate observed in schizophrenics seem to be a global trend. Research from Australia and Denmark confirmed a higher mortality rate among schizophrenic patients.
It is estimated that patients with schizophrenia tend to die 15-20 years earlier that the rest of the population. In one large cohort study conducted over 10 years, researchers found that there were more unnatural deaths than natural deaths, with suicide being the leading cause of death. They found that all-cause mortality was 4 times higher than the general population. They further broke this down to a 20 times higher rate of suicide, a 13 times higher death rate due to unnatural causes, and a 2 times higher rate due to natural causes.
Another study examines the higher mortality in schizophrenic patients due to cardiovascular disease. They estimate this mortality rate in these patients to range from 40-50%. They cite several causes of this observation. Schizophrenic patients have a higher prevalence of metabolic syndrome (MetS). In their study, they found 35% of males and 50% of females had MetS. These patients have a higher incidence of type 2 diabetes mellitus. While some speculate that this can be due to the use of anti-psychotic medications, a similar increase in the prevalence of T2DM was observed in young patients not taking any anti-psychotic medication. It was also observed that schizophrenic have a 3 times higher rate of smoking than the general population, and they tended to smoke more. In a Finnish study, the presence of smoking plus diabetes were the most important predictors of 8 year mortality in schizophrenia patients. Sedentary lifestyle is typical and only 26% of these patients meet weekly exercise recommendations. These patients also tend to eat unhealthy diets. Additionally, these patients tend to be unemployed and poor. Finally, some genetic factors appear to play a role in the increased prevalence of cardiovascular disease observed in schizophrenics. It has been discovered that there are many genes overlapping both diseases.
Despite the differing study results found, it is clear that schizophrenic patients die at much earlier ages from both natural and unnatural causes. While there are many lifestyle factors that are observed to play a role, genetic factors are still being discovered. It is also worth noting that for many of these patients, access to healthcare is a critical problem. Many of them are unemployed because of their disease and getting mental healthcare services difficult because of their insurance or lack of it. Also, many stigmas exist around this disease that makes people reluctant to seek help in the first place. Many medications used to treat psychosis have side effects which make the patient stop taking them. While treating the symptoms of schizophrenia are difficult, diagnosing and treating the comorbid conditions are even more so. Unless clinicians recognize and address the early mortality these patients suffer, increased death rates will continue and these patients lose many years of life. More studies need to be done to explore possible genetic links between schizophrenia and other diseases.
About the Author
Linda Girgis MD, FAAFP is a family physician practicing in South River, New Jersey and Clinical Assistant Professor at Rutgers Robert Wood Johnson Medical School. She was voted one of the top 5 healthcare bloggers in 2016. Follow her on twitter @DrLindaMD.