Currently, the guidelines around prostate cancer for physicians like me follow are murky, and best practices are subject to debate by different medical organizations. A widely-known recommendation called a PSA (Prostate Specific Antigen) screening, for example, has been fraught with failings and blamed for causing an unacceptable number of unnecessary prostate biopsies. On March 19, 2018, the results of the long-awaited PRECISION (Prostate Evaluation for Clinically Important Disease: Sampling Using Imaging Guidance or Not?) study were first published in the New England Journal of Medicine (NEJM). This study breaks new ground, and helps doctors find our way out of the recommendation crossfire.
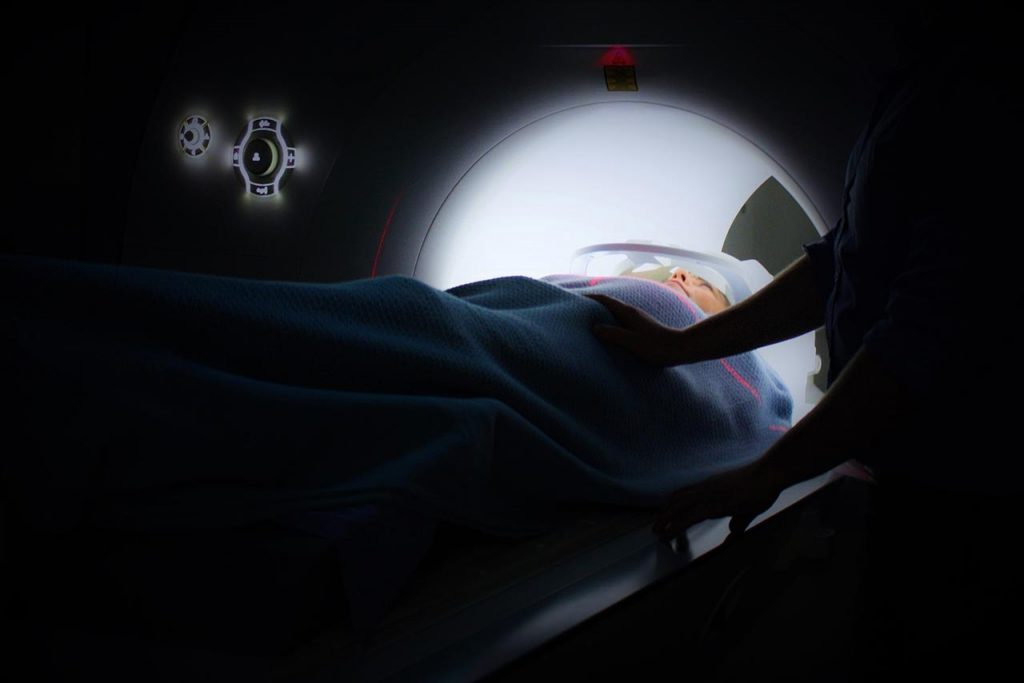
The PRECISION study was conducted in 25 medical centers in 11 different countries. The subjects were assigned, using a computer-generated randomization process, to either the MRI- targeted biopsy group or the standard-biopsy group. Subjects were referred from medical centers if there was suspicion of prostate cancer based on elevated PSA level and/or digital rectal exam findings. They were excluded if they had a previous prostate biopsy.
Five hundred men were evaluated from February 2016 through August 2017. Clinically significant cancer was found in 38% of the MRI-targeted biopsy group as opposed to 26% in the standard-biopsy group. Interestingly, MRI with or without biopsy, was found to be superior at the 95% confidence interval. Additionally, in the MRI-targeted biopsy group, fewer men were diagnosed with clinically insignificant cancers (9%) as compare to the standard-biopsy group (22%).
While both groups of men reported similar levels of discomfort immediately following the procedure, there were fewer complications in the MRI-targeted biopsy group at 30 days post-procedure. The results of the PRECISION trial reflect findings of some previous studies, although other results have historically been heterogeneous. What makes this study a particularly important is that it was conducted internationally with a large sample size. Additionally, they included centers that used their own testing resources and clinicians, reflecting real-world conditions.
For years, physicians have been left with substandard screening tests for the detection of prostate cancer. This study clearly provides an additional tool in determining the aggressiveness of a tumor that measuring PSA levels never could. Also, using MRI-targeted biopsies increases the accuracy of risk stratifying tumors and identifying clinically insignificant cancers that don’t need further treatment. This is a step in the right direction.
That said, it shows us just how much work there is left to be done. Perhaps the thing the PRECISION trial shows us we most need more research on is a completely non-invasive diagnostic test to establish significant prostate cancers that need further evaluation and treatment. Until we have that tool, biopsies will continue to be needed and used – whether or not everyone believes they are necessary.
About the Author
Linda Girgis MD, FAAFP is a family physician practicing in South River, New Jersey and Clinical Assistant Professor at Rutgers Robert Wood Johnson Medical School. She was voted one of the top 5 healthcare bloggers in 2016. Follow her on twitter @DrLindaMD.