The Alliance for Continuing Education in the Health Professionals hosted a Call for Submissions of high-quality outcome-based programs that effectively reported on the measured impact of educational initiatives that resulted in improvements in quality of patient care, behavior change, and/or HCP knowledge and competency.
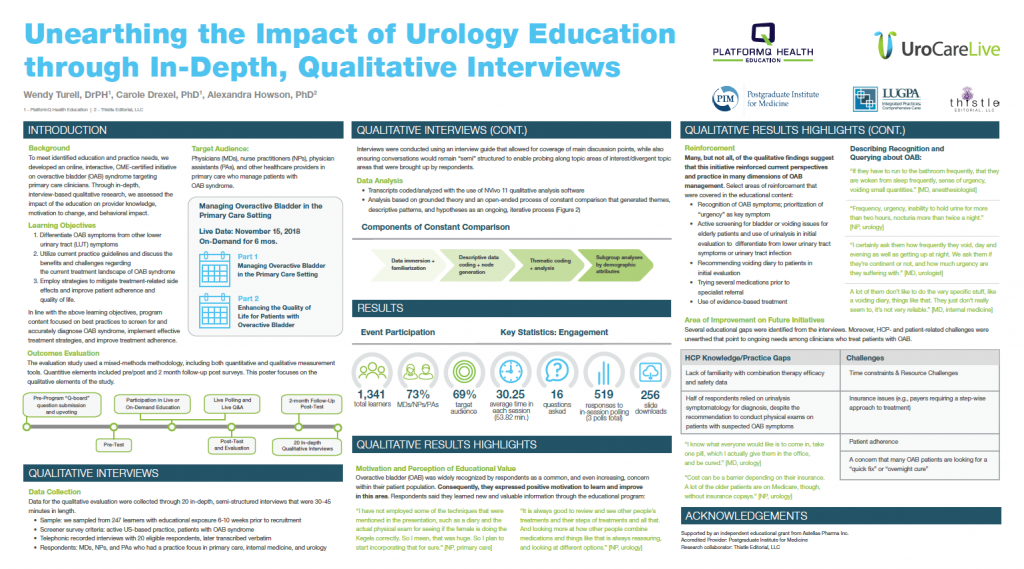
At the 2021 Virtual Alliance Industry Summit, PlatformQ Health’s outcomes poster, “Unearthing the impact of Urology education through in-depth, qualitative interviews” was among the group of recipients of the Best-in-Class Award. The poster highlights qualitative research – an underutilized element in the toolbox of evaluators in the continuing education for the health professions.
Watch a virtual presentation from the AIS virtual conference of the awarded poster, given by Wendy Turell, DrPH, CHCP, FACEHP, poster author and Vice President of CME Outcomes and Analytics at PlatformQ Health Education.
Where it started: A digital CME initiative in OAB
The award recognizes the results from an online, interactive CME certified initiative on overactive bladder syndrome (OAB) targeting primary care clinicians. Through in-depth, interview based qualitative research, the outcomes team assessed the impact of the education on provider knowledge and self-efficacy, identifying 4 key themes: 1. Taking OAB seriously; 2. Variations in therapy; 3. Patient motivations; 4. Education value.
The 60-minute CME activity, “Managing Overactive Bladder in the Primary Care Setting,” was accredited by the Postgraduate Institute for Medicine, produced in partnership with the Large Urology Group Practice Association and supported by an unrestricted educational grant from Astellas. The activity was designed to provide an overview of best practices for patient management in OAB syndrome, including recent clinician safety and efficacy data for therapeutic agents.
Activity Attendance Highlights
- 1,341 unique learners, 73% of whom were MDs, NPs, and PAs
- 519 responses to in-session polling
- 256 slide-set downloads
Reinforcing and improving practice
The activity addressed 3 learning objectives that also guided the focus of impact measurement. The evaluation methodology for this poster presentation focused on the qualitative portion of a mixed-methods evaluation; the full evaluation also included a survey-based quantitative approach, with pre, post and 2-month follow up measures.
The interview respondents, regardless of practice setting or specialty, described themselves as having extensive experience managing patients with OAB, and as being proactive with regards to managing OAB patients. The education validated current practices and provided new knowledge to HCP respondents regarding evaluation, initiating behavioral treatment, and combination therapy. Importantly, the qualitative findings suggest that the education reinforced current perspectives and practices.
Respondents expressed a positive motivation to learn about and improve their OAB care. Specifically, they reported learning valuable information about the following:
- Keeping their current practice and clinical approach up to date
- Integration of voiding diaries (OAB diagnostic/monitoring tools), as a tool for future use with patients
- Behavioral treatments that can be put into practice
- Combination therapies that can be integrated for those with persistent symptoms who need treatment escalation
Additionally, many of the qualitative findings suggest that this initiative reinforced current perspectives and practice in many dimensions of OAB management. More than half of participants described recently approved OAB treatments as their “go-to” therapy “if insurance allows” and noted the successful results they have had with a newer treatment.
Uncovering educational gaps and challenges
There were several educational gaps identified from the conducted interviews. Respondents seemed to lack familiarity with efficacy and safety data concerning combinations therapies. Half of respondents relied on urinalysis symptomatology for diagnosis, despite the recommendation to conduct physical exams on patients with suspected OAB symptoms.
The activity learners described a series of challenges, including time constraints that limited the capacity for providers to educate their patients, insurance issues, patient adherence, the presence of comorbidities, lack of resources, patient desire for a “quick-fix,” and patient embarrassment. These gaps and challenges can be focused on in future educational efforts and some can be directly addressed with direct-to-patient educational programs, or via resources provided to patient by HCPs.
Behind the notable methodology
The combination of quantitative and qualitative methods in healthcare allows for comprehensive evaluations of experience and change. The outcomes team can draw value from quantitative research, including statistical validity and the ability to generalize from conclusions, as well as from qualitative research, through depth of understanding and the acknowledgement of context.
Qualitative research methods (QRMs) allow for the collection of rich, descriptive data that illustrate learner change and the experience of HCPs treating illnesses. QRMs help researchers move beyond the “what” to understand the process of change and the “where, how, and under what circumstances” that lead to specific educational outcomes.